High dose HBO2 Ineffective for Post Concussion Syndrome
The U.S. Air Force, along with partners from McGuire Veterans Affairs Medical Center and U. S. Army Medical Research and Material Command, announced the results of the first ever randomized, placebo-controlled trial of hyperbaric oxygen to treat symptoms and cognitive impairments resulting from concussions or mild traumatic brain injury Oct. 16.
The pilot study, released to the public on the Journal of Neurotrauma website, demonstrated that high doses of hyperbaric oxygen 2.4 atmospheres absolute, or ATA, given daily over six weeks showed no added benefit in symptom relief of mTBI or post traumatic stress disorder symptoms over a group receiving a sham therapy consisting of breathing room air in the chamber under mild pressure (1.3 ATA).
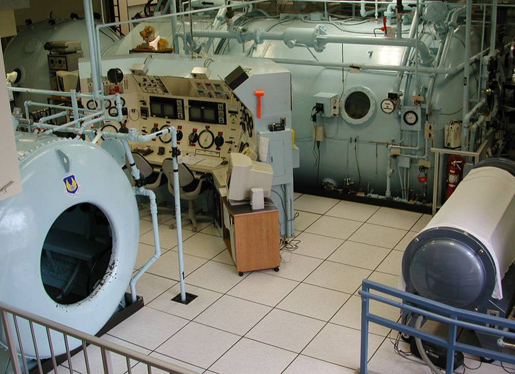
Hyperbaric oxygen, often abbreviated HBOT or HBO2, is a drug treatment in which a patient breathes oxygen under pressure to achieve elevated oxygen levels in the blood and tissue for a period of time. It is an approved therapy for 14 medical conditions, including non-healing diabetic wounds and carbon monoxide poisoning, at pressures ranging from 2.0 to 3.0 ATA. Although it has not been approved for TBI, anecdotes and small case studies have suggested a possible benefit for service members with post concussion syndrome and PTSD when using HBO2 at 1.5 ATA. A review of HBO2 and TBI by the Agency for Healthcare and Research Quality in 2003 suggested TBI research studies should look at hyperbaric oxygen in a dose response fashion.
This study was conducted at the U.S. Air Force School of Aerospace Medicine in San Antonio from 2009 to 2011 involving wounded service members still on active duty, who were still symptomatic three to 71 months after their TBI injury. Volunteers were recruited from military hospitals and flown to San Antonio for eight weeks to receive the intensive study intervention.
The 2.4 ATA dose of HBO2 selected was based on clinical observations that TBI symptoms improved while a service member was receiving standard hyperbaric therapy to assist in healing a traumatic jaw wound. According to Dr. George Wolf, a study investigator, participation in the study resulted in symptoms improvement in about 80% volunteers. However, those receiving oxygen showed no statistical improvements above the control or non-treatment arm. This higher dose of HBO2 was safely administered to and well-tolerated by the service members suffering from TBI symptoms. This pilot study infers that 2.4 ATA is not the optimal treatment dose.
This study is the first of four randomized clinical trials being conducted by a Department of Defense/Veteran Affairs consortium assembled to evaluate rigorously the potential for hyperbaric oxygen in the treatment of TBI.
"The lack of benefit in this study may be due to dose selected, as many experts have argued a lower dose (1.5 ATA) may be superior, and alternate doses are now under investigation," said Col. Scott Miller, director of the HBO2 Project Management Office at the U.S. Army Medical Materiel Development Activity and the physician leading the coordinated research effort.
Two additional clinical trials which are designed to examine those alternate regimens are nearing completion, with results expected within the year. These studies are also evaluating alternate ways to administer the placebo dose to evaluate whether the slightly pressurized air in the sham design may have contributed to any of the improvement.
This study was primarily funded by the U.S. Air Force Medical Support Agency Medical Modernization Directorate and the 711th Human Performance Wing, with additional support of the U.S. Navy Bureau of Medicine and Surgery and the USAMRMC.













